Abstract
Introduction: Antiplatelet antibody (APA) testing is considered an adjunct laboratory test in the diagnosis of immune thrombocytopenia (ITP). While it is not routinely obtained owing to inconsistent sensitivity and specificity in prior studies (Neunert et al, 2011), the definition of ITP used in these studies was not standardized. Additionally, potential clinical utility of this testing beyond diagnosis has been suggested, such as correlations between certain serologic patterns and response to IVIG (Peng et al, 2014). In consideration of these prior findings, we undertook a retrospective analysis of APA testing [glycoprotein-specific testing done by the commercial PakAuto assay (Immucor, Brookfield, WI), a monoclonal antibody immobilization of platelet antigens (MAIPA) assay, with all testing performed by the same laboratory] utilizing standardized ITP and Evans syndrome (ES) diagnostic criteria for patient inclusion. We examined serologic evolution over time and relation of antibody positivity to disease severity and response to therapies.
Methods: Data collected for analysis included dates and results of APA testing (including disease status and platelet count at time of testing), patient demographics, and disease characteristics. Satisfaction of the 2011 American Society of Hematology (ASH) ITP diagnostic criteria were required for ITP patient inclusion and standard definitions of disease severity and response to treatment from the ASH guidelines were used in analysis. Logistic regression was used to model the probability of disease severity (non-severe, severe, or refractory) and treatment response (to corticosteroids or IVIG) based on serologic findings. Longitudinal serologic evolution in patients with multiple APA assays were analyzed.
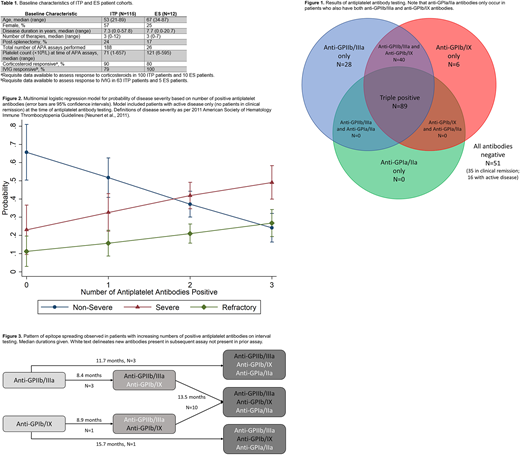
Results: A total of 214 APA assays from 115 ITP patients and 12 ES patients were collected; results from eluate testing (direct assay) only were used in analysis. Baseline patient characteristics are listed in Table 1. Of 7 possible positive test serologic patterns, only 4 were seen (Figure 1); antibodies against both GPIIb/IIIa and GPIb/IX were required for the presence of antibodies against GPIa/IIa. A multinomial logistic regression model including disease severity, age, sex, duration of disease, and platelet count at time of APA assay found a statistically significant predictive relationship between an increasing number of positive antibodies and disease severity [relative to non-severe ITP, relative risk ratio for severe ITP and refractory ITP was 1.89 (P=0.001) and 2.38 (P=0.004), respectively, per one additional positive antibody, Figure 2]. Multiple logistic regression models including antibody positivity to each platelet glycoprotein (GPIIb/IIIa, GPIb/IX, or GPIa/IIa), age, sex, disease duration and splenectomy status found a significant predictive relation between presence of anti-GPIa/IIa and non-response to corticosteroid treatment (odds ratio, 0.082, P=0.008). No significant relation was found between an antibody and non-response to IVIG. Fifty patients had multiple (2 to 5) APA assays performed over months to years. In evaluation of serologic evolution over time, all 7 patients who entered clinical remission also converted from a positive to a negative serology; 22 patients had stable serologic findings over time; 5 patients had a reduction in number of positive antibodies; and 18 patients demonstrated evidence for epitope spreading, with an increase in the number of positive antibodies (Figure 3). The sensitivity of a positive APA assay for the presence of active ITP was 91%. The sensitivity and specificity of a negative APA assay for remission in a patient with previously confirmed ITP (N=40 assays in patients with clinical remission in the study) were 88% and 91%, respectively.
Conclusions: The MAIPA-based direct APA assay is sensitive for the presence of active ITP in patients satisfying 2011 ASH diagnostic criteria. To our knowledge, this is the first study demonstrating that a higher number of positive glycoprotein-specific antibodies may predict for more severe disease as defined by 2011 ASH disease severity criteria. Anti-GPIa/IIa antibodies only occur in the setting of pre-existing positivity for both anti-GPIIb/IIIa and anti-GPIb/IX antibodies, possibly due to a distinctive sequence of epitope spreading. Serologic testing typically turns negative when a patient enters clinical remission.
Al-Samkari:Agios: Consultancy. Kuter:Novartis: Consultancy; Pfizer: Consultancy; Syntimmune: Consultancy; Argenx: Consultancy; Dova Pharmaceuticals: Consultancy, Membership on an entity's Board of Directors or advisory committees; ONO: Consultancy; Amgen Inc.: Consultancy; Bioverativ: Consultancy, Research Funding; Principia: Research Funding; Rigel: Consultancy, Research Funding; BMS: Research Funding; Protalex: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal